Heart Block
심장 차단
source-Yahoo
Heart block is a problem with your heartbeat signal moving from the upper to lower part of your heart. The signal can only get through sometimes, or not at all. This makes your heart beat slowly or skip beats. People with second-degree or third-degree heart block may experience fainting, tiredness and shortness of breath.
Overview
What is heart block?
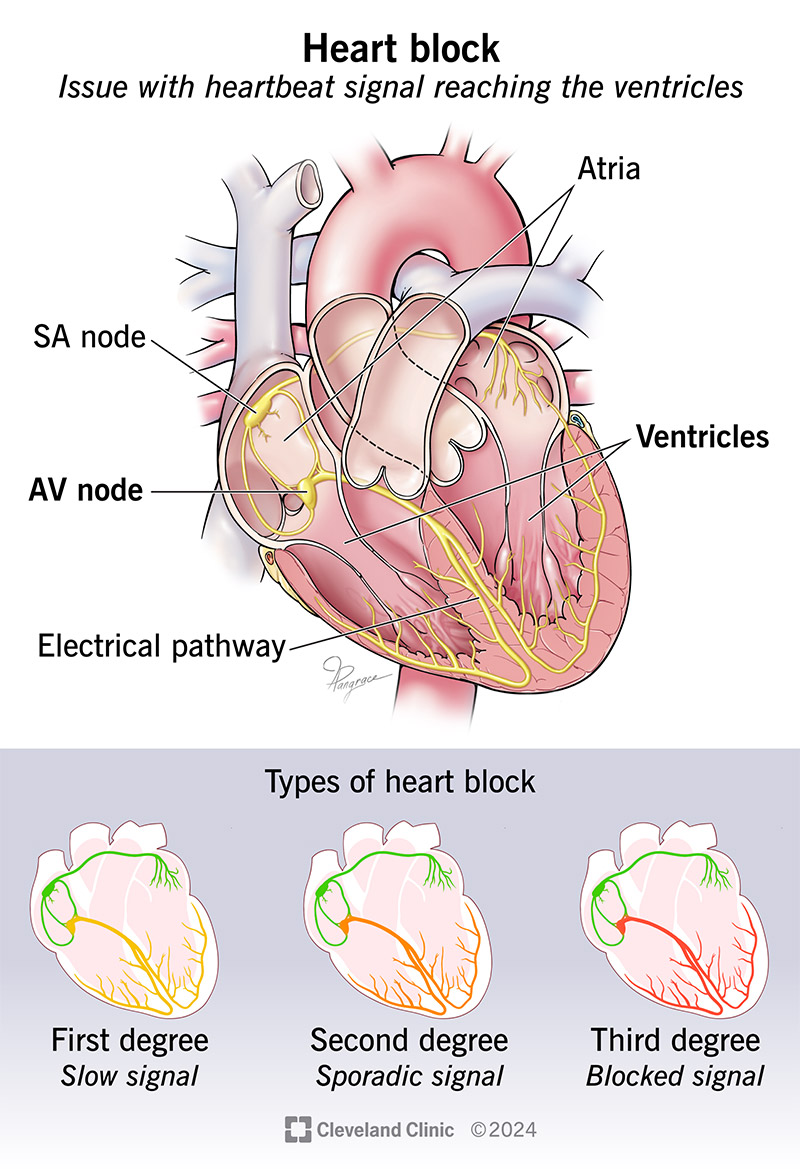
Heart block is an issue with a heartbeat signal traveling from the top chambers of your heart to the bottom chambers of your heart. Normally, electrical signals (impulses) travel from your heart’s upper chambers (atria) to your lower chambers (ventricles). The signal moves through your AV node, a cluster of cells that link the electrical activity from your top to bottom chambers. If you have heart block, the signal only makes it to your ventricles some of the time, if at all.
The result is a heart that may not work well. Your heart may beat slowly or skip beats. In severe cases, heart block can affect your heart’s ability to pump blood, causing low blood flow to your entire body.
People are more likely to acquire heart block later in life than to have it at birth.
Other names for heart block are atrioventricular (AV) block or a conduction disorder.
Types of heart block
Heart blocks can range from mild to severe, depending on whether the electrical signal can get through, and how often. Heart block types are:
First-degree heart block: The electrical impulse still reaches your ventricles, but moves more slowly than normal through the AV node. This is the most mild type of heart block.
Second-degree (incomplete) heart block: With this type, your heart’s impulses only get to the lower chambers some of the time. The types of second-degree heart block are:
- Type I, also called Mobitz Type I or Wenckebach’s AV block: This is a less serious form of second-degree heart block. The electrical signal gets slower and slower until your heart actually skips a beat.
- Type II, also called Mobitz Type II: While most of the electrical signals reach your ventricles, every so often, some don’t. Your heartbeat becomes irregular and slower than normal. This form of second-degree heart block is more serious and may warrant a pacemaker.
Third-degree heart block: This is a complete blockage of the electrical signal from your atria to your ventricles. Third-degree block negatively affects your heart’s ability to pump blood out to your body. This form of heart block is serious and usually requires a pacemaker for treatment.
Symptoms and Causes
What are the symptoms?
Symptoms of heart block vary depending on the severity of the block and how it affects the heart pump.
Heart block symptoms may include:
- Chest pain.
- Tiredness.
- Shortness of breath.
- Heart palpitations.
- Rapid breathing.
- Nausea.
- Dizziness.
- Fainting.
People with first-degree heart block may not have any symptoms. A provider may find first-degree heart block during a routine electrocardiogram (EKG).
Symptoms of third-degree heart block are more intense due to the slow heart rate. If you have severe symptoms, get medical attention right away.
What causes heart block?
Causes of heart block include:
- Heart attack.
- Coronary artery disease (CAD).
- Heart muscle disease (cardiomyopathy).
- Heart valve diseases.
- Scarring in your conduction system from an unknown cause.
- Issues with your heart’s structure (since birth).
- Heart damage during open heart surgery.
- Medication side effects (from beta-blockers, digitalis and calcium channel blockers).
- Exposure to toxins.
- Obstructive sleep apnea.
- Thyroid disease.
- Infections like Lyme disease.
- Autoimmune diseases.
- Genetic anomalies.
What are the risk factors for heart block?
You may be at an increased risk of a heart block if:
- You have other heart conditions like coronary artery disease or heart valve disease.
- You’ve had abnormalities in your heart since birth.
- You have a disease (like rheumatic heart disease or sarcoidosis) that affects your heart.
- You have an overactive vagus nerve that causes your heart to slow down.
- You take medications that make your heart’s electrical impulses move more slowly. These drugs may include heart and blood pressure medications (beta-blockers, diuretics, calcium channel blockers, digoxin), antiarrhythmics, muscle relaxants, sedatives, antidepressants and antipsychotics.
What are the complications of heart block?
The complications can be life-threatening and include:
- Heart failure.
- Arrhythmia (irregular heartbeat).
- Heart attack.
- Sudden cardiac arrest.
Diagnosis and Tests
How is heart block diagnosed?
To diagnose heart block, your healthcare provider will:
- Review your medical history.
- Review your biological family’s health history.
- Ask questions about your overall health, eating habits, physical activity level and symptoms.
- Ask you about any medications you’re taking (prescription or over the counter).
- Ask you if you smoke or use recreational drugs.
- Listen to your heart and check your heart rate.
- Check for signs of heart failure, like fluid buildup in your feet, ankles and legs.
Your cardiologist may refer you to an electrophysiologist, an expert in the electrical activity of your heart.
What tests will be done to diagnose heart block?
Tests you might have include:
- Blood tests.
- Genetic tests.
- Electrocardiogram (EKG).
- Ambulatory monitor.
- Loop recorder.
- Electrophysiology study.
- Exercise stress test.
Management and Treatment
How is heart block treated?
Heart block treatment varies from person to person. A provider may admit you to the hospital to monitor your heart. To manage your condition, your cardiologist will consider:
- Which type of heart block you have.
- The severity of your heart block.
- How it affects your heart’s ability to function.
- The symptoms you’re having.
Sometimes, making changes to medicines or treatment for heart disease stops heart block. Other people may need a temporary or permanent pacemaker that sends electrical pulses to their hearts.
- First-degree block: You probably won’t need treatment.
- Second-degree block: You may not need treatment if you have Type 1. If you have symptoms, you may need a temporary or permanent pacemaker to keep your heart beating like it should.
- Third-degree block: People with this type almost always need a pacemaker.
If you need a pacemaker, your provider will talk to you about the details, the type that’s best for you, and what to expect before, during and after you get your pacemaker.
Complications/side effects of the treatment
If you receive a temporary or permanent pacemaker, you may have side effects like:
- Issues with the device’s programming.
- Device malfunctions.
- Infection.
- Blood clots.
- Injury to your heart.
How long does it take to recover from this treatment?,
you may need to stay overnight in the hospital. You should be able to get back to your regular activities a few days to weeks after surgery. Ask your provider for specific restrictions after the procedure.
Prevention
Can heart block be prevented?
You may be able to prevent some causes of heart block, like heart disease.
Steps you can take to keep your heart and body as healthy as possible include:
- Lead a heart-healthy lifestyle. This includes eating heart-healthy foods, getting regular physical activity, getting enough sleep each night, reducing stress, limiting alcohol and avoiding smoking and recreational drugs.
- Talk with your provider about medications and other supplements you take. They can review what you’re taking to find out if any of them change the normal levels of certain substances in your body. (Potassium, calcium and magnesium play a role with your heart’s electrical system.) Your provider can change your medication to a different drug class if needed.
Outlook / Prognosis
What can I expect if I have heart block?
If you have first-degree heart block, ask your cardiologist or electrophysiologist what — if any — changes you need to make to your lifestyle or medications. This type of heart block doesn’t usually get in the way of your normal activities.
In general, a pacemaker won’t seriously restrict your ability to take part in sports and leisure activities. It’s important to follow your provider’s instructions for pacemaker monitoring so they can ensure your device is working correctly.
How long heart block lasts
The cause of your heart block determines how long it lasts. If you replace a medication that causes heart block, that can resolve the issue. But heart block from another cause will likely be a lifelong condition.
Outlook for heart block
Heart blocks can be serious. Without treatment, severe heart block can cause sudden cardiac arrest. But most commonly, untreated heart block can cause lightheadedness or fainting spells.
With treatment, your outlook depends on your age and what other conditions you have.
Living With
How do I take care of myself?
If you have a pacemaker:
- Avoid close contact with magnetic devices and any device that sends out an electrical field. This includes staying at least 6 inches from cell phones.
- For example, don’t keep your cell phone in your shirt pocket.
- When going through security screening stations (like airports and courthouses), tell the screeners that you have a pacemaker and should avoid the handheld wands.
- Always carry a card that states the type of pacemaker you have.
- Tell all your healthcare providers and your dentist that you have a pacemaker.
- Some medical procedures, like magnetic resonance imaging (MRI), can interfere with pacemakers. A provider may need to reprogram your pacemaker after certain kinds of surgery.
When should I see my healthcare provider?
If you have a pacemaker, your cardiologist will want to check it periodically to make sure that it continues to work well. They can monitor you remotely, but you’ll need annual in-person appointments when your provider evaluates and adjusts your pacemaker.
Call your healthcare provider if you experience:
- Dizziness or fainting.
- Chest pain.
- Racing heartbeat or skipped heartbeat.
- Weakness.
- Shortness of breath.
- Swollen feet, ankles or legs.
When should I go to the ER?
You need immediate medical care if you have a heart attack or cardiac arrest. Let your family and co-workers know about your risk of these (and the symptoms) so they can call 911 or your local emergency number.
What questions should I ask my doctor?
Questions to ask your healthcare provider may include:
- What type of heart block do I have?
- Do I need treatment?
- Which kind of treatment is best for me?
- If my child has heart block from birth, will my future children have it at birth, too?
A note from Cleveland Clinic
It can be unnerving to have chest pain or have trouble catching your breath. But getting a heart block diagnosis can explain why you’re experiencing those symptoms. The good news is that people who need treatment can have success with medicines or pacemakers that keep their hearts in a normal rhythm. Be sure to ask your provider about anything that isn’t clear when discussing your treatment plan
심장 차단
source-yahoo
심장 차단은 심장 박동 신호가 심장의 윗부분에서 아랫부분으로 이동하는 데 문제가 있는 것입니다.
신호는 가끔만 전달되거나 전혀 전달되지 않습니다.
이로 인해 심장이 느리게 뛰거나 박동이 뜁니다.
2도 또는 3도 심장 차단이 있는 사람은 실신, 피로, 호흡 곤란을 경험할 수 있습니다.
내용 개요 증상 및 원인 진단 및 검사 관리 및 치료 예방 전망/예후 생활
개요
심장 차단이 있는 경우 심실에 전달되는 심장 박동 신호가 느리거나 신뢰할 수 없거나 완전히 차단될 수 있습니다.
심장 차단은 심장 박동 신호가 제때, 매번 또는 전혀 심장의 아랫부분에 도달하지 못하게 합니다.
심장 차단이란 무엇입니까?
심장 차단은 심장의 윗부분에서 아랫부분으로 심장 박동 신호가 이동하는 문제입니다.
일반적으로 전기 신호(임펄스)는 심장의 윗부분(심방)에서 아랫부분(심실)으로 이동합니다.
신호는 전기적 활동을 위쪽에서 아래쪽 챔버로 연결하는 세포 클러스터인 AV 노드를 통해 이동합니다.
심장 차단이 있는 경우 신호는 심실에 도달하는 경우가 거의 없거나 전혀 없습니다.
그 결과 심장이 제대로 작동하지 않을 수 있습니다.
심장이 느리게 뛰거나 박동을 건너뛸 수 있습니다.
심각한 경우 심장 차단은 심장의 혈액 펌핑 능력에 영향을 미쳐 전신으로의 혈류가 감소할 수 있습니다.
사람들은 태어날 때보다 나중에 심장 차단을 받을 가능성이 더 큽니다.
심장 차단의 다른 이름으로는 심방실(AV) 차단 또는 전도 장애가 있습니다.
심장 차단의 유형
심장 차단은 전기 신호가 통과할 수 있는지 여부와 빈도에 따라 경미한 것에서 심각한 것까지 다양합니다.
심장 차단 유형은 다음과 같습니다.
1도 심장 차단: 전기적 충동이 여전히 심실에 도달하지만 AV 노드를 통해 정상보다 느리게 이동합니다. 이것은 가장 가벼운 유형의 심장 차단입니다.
2도(불완전) 심장 차단: 이 유형의 경우 심장의 충동은 때때로만 하부 챔버에 도달합니다. 2도 심장 차단의 유형은 다음과 같습니다.
1형, Mobitz 1형 또는 Wenckebach의 AV 차단이라고도 함: 이것은 2도 심장 차단의 덜 심각한 형태입니다. 전기 신호는 심장이 실제로 박동을 건너뛸 때까지 점점 더 느려집니다.
2형, Mobitz 2형이라고도 함: 대부분의 전기 신호가 심실에 도달하지만 가끔은 그렇지 않습니다. 심장 박동이 불규칙하고 정상보다 느려집니다. 이 2도 심장 차단의 형태는 더 심각하며 페이스메이커가 필요할 수 있습니다.
3도 심장 차단: 이것은 심방에서 심실로 가는 전기 신호가 완전히 막힌 것입니다. 3도 차단은 심장이 신체로 혈액을 펌핑하는 능력에 부정적인 영향을 미칩니다. 이 형태의 심장 차단은 심각하며 일반적으로 치료를 위해 페이스메이커가 필요합니다.
증상 및 원인
증상은 무엇입니까?
심장 차단 증상은 차단의 심각도와 심장 펌프에 미치는 영향에 따라 다릅니다.
심장 차단 증상은 다음과 같습니다.
흉통.
피로.
호흡 곤란.
심계항진.
호흡이 빨라짐.
메스꺼움.
현기증.
실신.
1도 심장 차단 환자는 증상이 없을 수 있습니다. 의료 제공자는 정기 심전도(EKG) 중에 1도 심장 차단을 발견할 수 있습니다.
3도 심장 차단의 증상은 심박수가 느려서 더 강렬합니다. 증상이 심하면 즉시 의료 지원을 받으십시오.
심장 차단의 원인은 무엇입니까?
심장 차단의 원인은 다음과 같습니다.
심장 마비.
관상 동맥 질환(CAD).
심장 근육 질환(심근병).
심장 판막 질환.
알 수 없는 원인으로 인한 전도계의 흉터.
심장 구조 문제(출생 이후).
개심 수술 중 심장 손상.
약물 부작용(베타 차단제, 디지탈리스 및 칼슘 채널 차단제).
독소 노출.
폐쇄성 수면 무호흡증.
갑상선 질환.
라임병과 같은 감염.
자가면역 질환.
유전적 이상.
심장 차단의 위험 요인은 무엇입니까?
다음과 같은 경우 심장 차단 위험이 증가할 수 있습니다.
관상 동맥 질환이나 심장 판막 질환과 같은 다른 심장 질환이 있는 경우.
선천적으로 심장에 이상이 있는 경우.
심장에 영향을 미치는 질환(류마티스성 심장 질환이나 육아종증 등)이 있는 경우.
심장이 느려지는 과활성 미주신경이 있는 경우.
심장의 전기적 자극을 더 느리게 만드는 약물을 복용하는 경우. 이러한 약물에는 심장 및 혈압 약물(베타 차단제, 이뇨제, 칼슘 채널 차단제, 디곡신), 항부정맥제, 근이완제, 진정제, 항우울제 및 항정신병제가 포함될 수 있습니다.
심장 차단의 합병증은 무엇입니까?
합병증은 생명을 위협할 수 있으며 다음을 포함합니다.
심부전.
부정맥(불규칙한 심장 박동).
심장 마비.
갑작스러운 심장 마비.
진단 및 검사
심장 차단은 어떻게 진단합니까?
심장 차단을 진단하기 위해 의료 서비스 제공자는 다음을 수행합니다.
병력을 검토합니다.
친가족의 건강 기록을 검토합니다.
전반적인 건강, 식습관, 신체 활동 수준 및 증상에 대해 질문합니다.
복용 중인 약물(처방전 또는 일반 의약품)에 대해 질문합니다.
흡연 또는 오락용 약물을 사용하는지 묻습니다.
심장 소리를 듣고 심박수를 확인합니다.
발, 발목 및 다리에 체액이 쌓이는 것과 같은 심부전 징후를 확인합니다.
심장 전문의는 심장의 전기적 활동을 전문으로 하는 전기 생리학자에게 의뢰할 수 있습니다.
심장 차단을 진단하기 위해 어떤 검사를 합니까?
받을 수 있는 검사는 다음과 같습니다.
혈액 검사.
유전자 검사.
심전도(EKG).
보행 모니터.
루프 레코더.
전기 생리학 연구.
운동 스트레스 검사.
관리 및 치료
심장 차단은 어떻게 치료합니까?
심장 차단 치료는 사람마다 다릅니다. 제공자는 심장을 모니터링하기 위해 병원에 입원시킬 수 있습니다. 귀하의 상태를 관리하기 위해 심장 전문의는 다음을 고려합니다.
귀하의 심장 차단 유형.
심장 차단의 심각도.
심장 기능에 미치는 영향.
나타나는 증상.
때때로 심장 질환에 대한 약물이나 치료를 변경하면 심장 차단이 중단됩니다. 다른 사람들은 심장에 전기 펄스를 보내는 일시적 또는 영구적 페이스메이커가 필요할 수 있습니다.
1도 차단: 치료가 필요하지 않을 가능성이 큽니다.
2도 차단: 1형이 있는 경우 치료가 필요하지 않을 수 있습니다. 증상이 있는 경우 심장이 정상적으로 뛰도록 일시적 또는 영구적 페이스메이커가 필요할 수 있습니다.
3도 차단: 이 유형의 사람들은 거의 항상 페이스메이커가 필요합니다.
페이스메이커가 필요한 경우 제공자는 세부 정보, 귀하에게 가장 적합한 유형, 페이스메이커를 받기 전, 받는 동안, 받은 후에 예상되는 사항에 대해 설명합니다.
합병증/치료 부작용
일시적 또는 영구적 심장 박동 조절기를 받는 경우 다음과 같은 부작용이 있을 수 있습니다.
장치 프로그래밍 문제.
장치 오작동.
감염.
혈전.
심장 손상.
이 치료에서 회복하는 데 얼마나 걸립니까?
심장 박동 조절기를 받은 후 밤새 병원에 머물러야 할 수 있습니다. 수술 후 며칠에서 몇 주 후에 정상적인 활동으로 돌아갈 수 있어야 합니다. 시술 후 특정 제한 사항에 대해 의료 제공자에게 문의하십시오.
예방
심장 차단을 예방할 수 있습니까?
심장 질환과 같은 일부 심장 차단 원인을 예방할 수 있습니다.
심장과 신체를 가능한 한 건강하게 유지하기 위해 취할 수 있는 단계는 다음과 같습니다.
심장 건강한 라이프스타일을 영위하십시오. 여기에는 심장 건강에 좋은 음식을 섭취하고, 규칙적인 신체 활동을 하고, 매일 밤 충분한 수면을 취하고, 스트레스를 줄이고, 알코올을 제한하고, 흡연과 오락용 약물을 피하는 것이 포함됩니다.
의료 제공자와 복용하는 약물 및 기타 보충제에 대해 상의하십시오. 그들은 당신이 복용하는 것을 검토하여 그 중 어떤 것이 신체의 특정 물질의 정상 수치를 변화시키는지 알아낼 수 있습니다. (칼륨, 칼슘 및 마그네슘은 심장의 전기 시스템과 역할을 합니다.) 필요한 경우 제공자가 귀하의 약을 다른 약물 계열로 변경할 수 있습니다.
전망/예후
심장 차단이 발생하면 어떤 일이 예상되나요?
1도 심장 차단이 있는 경우 심장 전문의 또는 전기 생리학자에게 생활 방식이나 약물을 어떻게 변경해야 하는지 물어보세요. 이 유형의 심장 차단은 일반적으로 정상적인 활동을 방해하지 않습니다.
일반적으로 페이스메이커는 스포츠 및 여가 활동에 참여하는 능력을 심각하게 제한하지 않습니다. 페이스메이커 모니터링에 대한 제공자의 지침을 따르는 것이 중요하여 장치가 올바르게 작동하는지 확인할 수 있습니다.
심장 차단이 지속되는 기간
심장 차단의 원인에 따라 지속 기간이 결정됩니다. 심장 차단을 유발하는 약물을 대체하면 문제가 해결될 수 있습니다. 그러나 다른 원인으로 인한 심장 차단은 평생 지속될 가능성이 높습니다.
심장 차단에 대한 전망
심장 차단은 심각할 수 있습니다. 치료하지 않으면 심각한 심장 차단이 갑작스러운 심장 마비를 일으킬 수 있습니다. 그러나 가장 흔하게 치료하지 않은 심장 차단은 현기증이나 실신을 일으킬 수 있습니다.
치료를 받으면 전망은 나이와 다른 질환에 따라 달라집니다.
생활
어떻게 하면 나 자신을 돌볼 수 있을까요?
심장 조율기를 사용하는 경우:
자석 장치 및 전기장을 방출하는 모든 장치와의 밀접한 접촉을 피하십시오. 여기에는 휴대전화에서 최소 6인치 거리를 두는 것이 포함됩니다.
예를 들어, 휴대전화를 셔츠 주머니에 넣지 마십시오.
보안 검색대(공항 및 법원 등)를 통과할 때 검색원에게 심장 조율기를 사용하고 있으며 손에 든 막대는 피해야 한다고 말하십시오.
항상 심장 조율기 유형을 명시한 카드를 휴대하십시오.
모든 의료 제공자와 치과 의사에게 심장 조율기를 사용하고 있다고 말하십시오.
자기 공명 영상(MRI)과 같은 일부 의료 시술은 심장 조율기에 영향을 미칠 수 있습니다. 제공자는 특정 종류의 수술 후 심장 조율기를 다시 프로그래밍해야 할 수 있습니다.
언제 의료 제공자를 만나야 합니까?
심장 조율기를 사용하는 경우 심장 전문의가 심장 조율기가 계속 잘 작동하는지 확인하기 위해 주기적으로 검사하고자 할 것입니다. 원격으로 모니터링할 수 있지만 제공자가 심장 조율기를 평가하고 조정할 때 매년 직접 방문해야 합니다.
다음과 같은 증상이 나타나면 의료 서비스 제공자에게 연락하세요.
현기증이나 실신.
흉통.
심장 박동이 빨라지거나 심장 박동이 건너뜀.
쇠약.
호흡 곤란.
발, 발목 또는 다리가 부음.
언제 응급실에 가야 합니까?
심장 마비나 심장 정지가 발생하면 즉각적인 치료가 필요합니다. 가족과 직장 동료에게 이러한 위험(및 증상)을 알려서 911이나 지역 비상 번호로 전화할 수 있도록 하세요.
의사에게 어떤 질문을 해야 합니까?
의료 서비스 제공자에게 물어봐야 할 질문은 다음과 같습니다.
어떤 유형의 심장 차단이 있습니까?
치료가 필요합니까?
어떤 종류의 치료가 나에게 가장 적합합니까?
내 아이가 태어날 때부터 심장 차단이 있는 경우 미래의 아이들도 태어날 때부터 같은 증상이 있습니까?
클리블랜드 클리닉의 메모
흉통이 있거나 숨을 쉬는 데 어려움이 있으면 불안할 수 있습니다. 하지만 심장 차단 진단을 받으면 이러한 증상이 나타나는 이유를 설명할 수 있습니다. 좋은 소식은 치료가 필요한 사람들이 심장을 정상적인 리듬으로 유지하는 약이나 페이스메이커로 성공할 수 있다는 것입니다. 치료 계획을 논의할 때 명확하지 않은 사항에 대해서는 반드시 제공자에게 물어보세요.
update 1/22/2025
Copyright drleepediatrics.com 2/2/2026